Scientists have mapped parts of Britain where there is a risk of transmission of tick-borne encephalitis virus, which has become a growing health problem in Europe.
In the past five years, there have been only a handful of cases of people here contracting the virus, which can cause flu-like symptoms and, in some cases, seizures or inflammation of the brain. However, changes in climate and land use could increase the risk in some places in coming years and the presence of deer, the primary hosts of adult ticks, is a crucial factor in driving tick numbers.
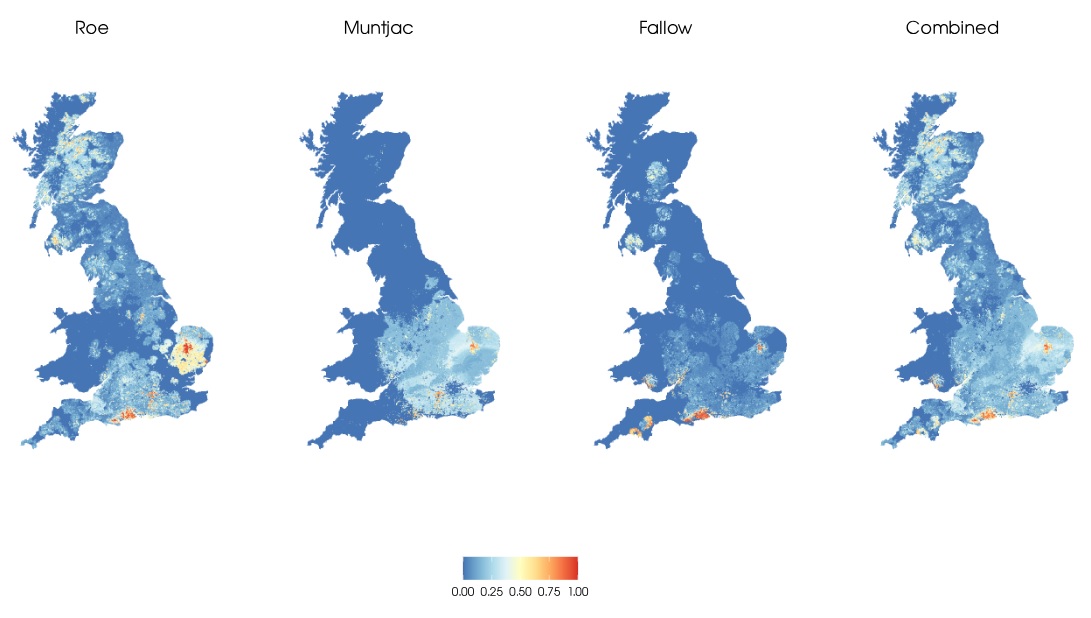
A study by the UK Centre for Ecology & Hydrology and the UK Health Security Agency found that deer are more likely to be exposed to tick-borne encephalitis virus (TBEV) through being bitten by infected ticks if an area has multiple deer species, high concentrations of coniferous woodland, and warmer winter and spring temperatures.
The immune system of deer fights off the virus before a full-blown infection develops, and this response can be measured from blood samples, making deer an ideal sentinel of where transmission of the virus is occurring across the UK
Landmark study
The scientists combined extensive UKHSA data on where deer were exposed to TBEV with information about local climate, land cover and recreational use. They produced high-resolution ‘risk maps’ that identified 1km x 1km areas where people may be exposed to TBEV across Britain. Areas of highest risk included the heavily forested areas of Hampshire, Dorset and East Anglia that have high deer numbers.
However, there are no reports of people contracting TBE around Thetford Forest on the Suffolk/Norfolk border, for example, despite one study finding almost half the deer surveyed there had been exposed to the virus. This demonstrates that even where there is a high risk of exposure whether this translates into human cases of tick-borne encephalitis will depend on local conditions and the complex interactions between people, the environment and wildlife.
Dr Richard Hassall of the UK Centre for Ecology & Hydrology (UKCEH), who led the research, explained: “This is the first study to investigate the environmental factors affecting the transmission of tick-borne encephalitis virus in the UK.
“We hope our risk maps can guide deer and tick surveillance by government agencies, and make the public, forest contractors, farmers and local health authorities more aware of the risks from TBE and other diseases transmitted by ticks.”
Varied factors influence risk
The presence of multiple deer species can increase tick numbers as deer are one of the main hosts that female adult ticks feed on before they lay eggs.
The researchers say warmer winter and spring temperatures could influence tick feeding patterns to facilitate the transmission and spread of the virus. Further studies are needed to better understand why coniferous woodland and the animals associated with these habitats may increase suitability for TBEV.
The study, published in the journal Eurosurveillance, was carried out as part of the ongoing TICKSOLVE project. The research team, from UKCEH, the UK Health Security Agency (UKHSA), the University of Liverpool and the University of Glasgow, is now investigating how afforestation and a warmer climate in Britain could increase tick activity and virus transmission.
Dr Maya Holding of UKHSA said: “This collaboration has enabled us to understand what environmental factors that might be driving at risk areas for TBEV, which is helping us target our surveillance programme in animals and humans and to raise awareness in at-risk areas."
Further information
Hassall et al. 2025. Identifying hotspots and risk factors for tick-borne encephalitis virus emergence at its range margins to guide interventions. Eurosurveillance. DOI: 10.2807/1560-7917.ES.2025.30.13.2400441. Open access.
About one in four people infected with the TBE virus develop symptoms, including high fever and severe headache, and up to a third of these sufferers have long-term complications from the disease, according to the European Centre for Disease Prevention and Control (ECDC). More serious symptoms can include seizures as well as encephalitis or meningitis.